SmarterDx is now proudly part of Smarter Technologies
LEARN MORE
Sicker patients, slimmer margins? A smarter solution: SmarterPrebill™ uses the differential diagnosis process to uncover missing billing codes and unlock hidden revenue and boost quality scores. By reviewing every patient’s complete record, SmarterPrebill ensures your hospital captures the full value of your care.
The result? New revenue. Better quality. Stronger margins. All without breaking a sweat.



Get 5:1 ROI starting on Day 1. Reconcile your clinical and billing data for every patient story and capture potentially millions in annual net new revenue. We’re talking an average of $2.5 million in realized annual net new revenue per 10,000 patient discharges.
Capture all of the correct diagnostic codes with evidence-based findings (this may include DRG downgrades). Our proprietary algorithms analyze your data automatically, but all findings are validated by your CDI team. That's what we like to call "peace of mind.”
Missing documentation details can misrepresent the patient’s true complexity and severity, lowering quality metrics like mortality and readmissions. Analyze the entire patient record to tell the most accurate patient story and secure the quality of care metrics your staff works so hard to earn.
Measuring ROI can often feel like guesswork with most health technologies. Not with SmarterPrebill: Our dynamic dashboards provide clear insights, from executive summaries of total revenue improvement to detailed breakdowns by location, case category, reviewing user, and more. Realizing real ROI has never been simpler.
Solutions that cost six figures or more before they’re even up and running are tough bets to make. With SmarterPrebill, results-based pricing means no risks, no upfront costs. You pay only for approved and billed findings. When you partner with us, you’re betting on a sure thing.
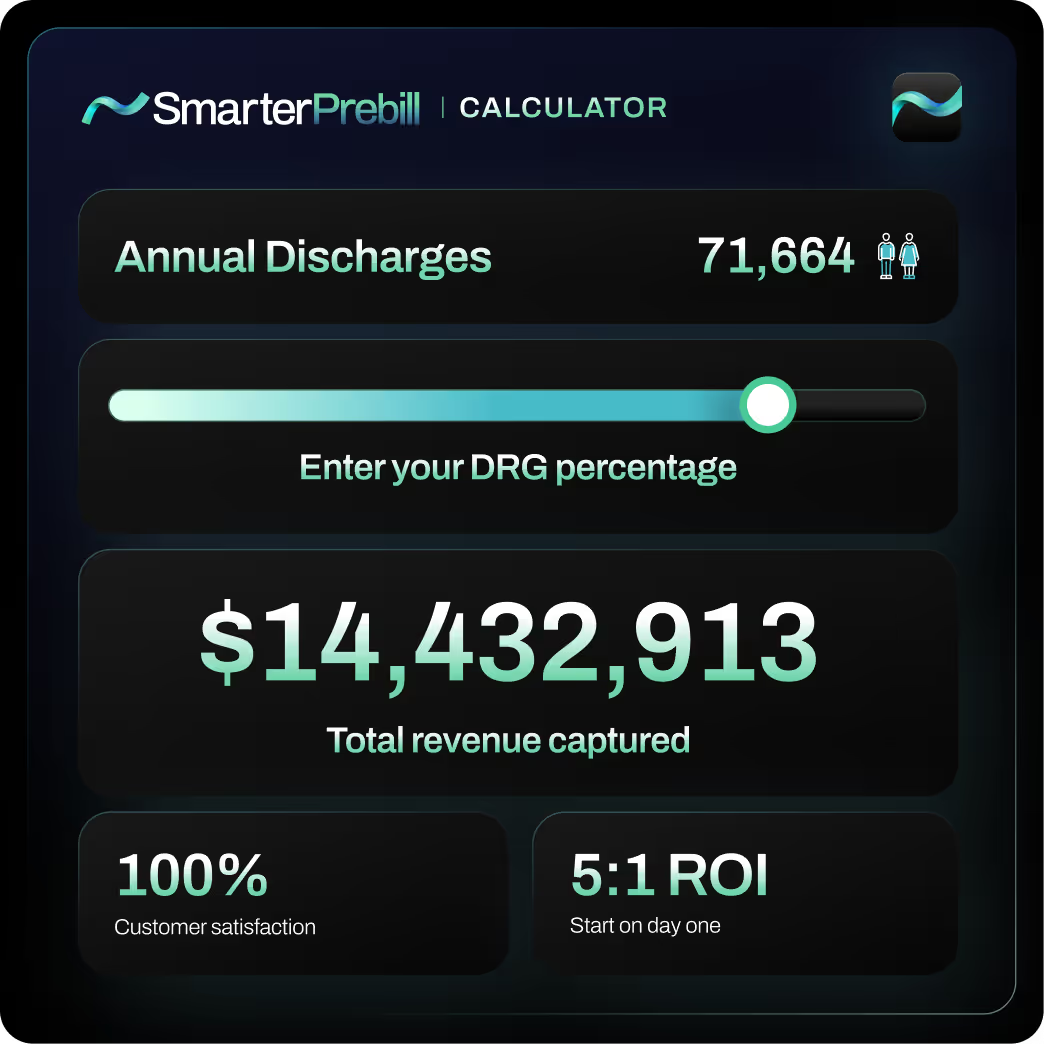
Every dollar counts in healthcare. So let us crunch the numbers to see how much net new revenue we could capture together.
Imagine your mission to capture missed or inaccurate diagnoses as an epic video game. You're racing to capture every opportunity — but it's overwhelming. With SmarterPrebill, you’re the main character, and our AI boosts your speed and precision, helping you capture even more revenue and quality opportunities.
_1_1.gif)
SmarterPrebill analyzes the entire patient record for every discharge. With more than 10,000 diagnoses and procedures identified by proprietary clinical algorithms, we capture everything, even things that were not documented in the notes. We're talking labs, meds, orders, vitals, and the results of radiology and pathology studies: Every data point within the 30K in the record.

Each of our recommendations includes the full clinical reasoning behind it, with all the relevant data from the record. Your CDI teams can see everything they need in one place, eliminating searches for backup and other manual administrative tasks.
Get tools to analyze total revenue improvement and impact per recommendation from every angle: location, service, DRG, provider, CDI reviewer and missing data-type, all the way down to case level. Continuously improve training and processes to ensure the quality and consistency of documenting and coding.


Implementation in weeks. Refreshing, right?
SmarterPrebill works seamlessly with your existing people, processes and technologies — no need to rip and replace. You can implement SmarterPrebill into your current workflow and tech stack in weeks and start seeing net new revenue on Day 1.
No matter your technology or program baseline, SmarterPrebill will deliver results to strengthen your financial health and quality scores.
Ready to learn more? Get in touch with us today and we’ll set you on the path to revenue integrity.