SmarterDx is now proudly part of Smarter Technologies
LEARN MORE
In healthcare, AI has become a major buzzword, and for good reason: It holds real potential to transform the industry.
AI healthcare market growth between 2019 and 2020
Projected AI market growth between 2024 & 2030
$32.3 Billion to
and not all are as powerful as the next. So, how do you separate fact from fiction in the CDI universe? Let’s explore what AI really means, how it’s being used in CDI, and debunk the top falsehoods with facts.

A simple definition
Algorithms that can perform tasks that require intelligence, like understanding languages, recognizing images, or making decisions using data.

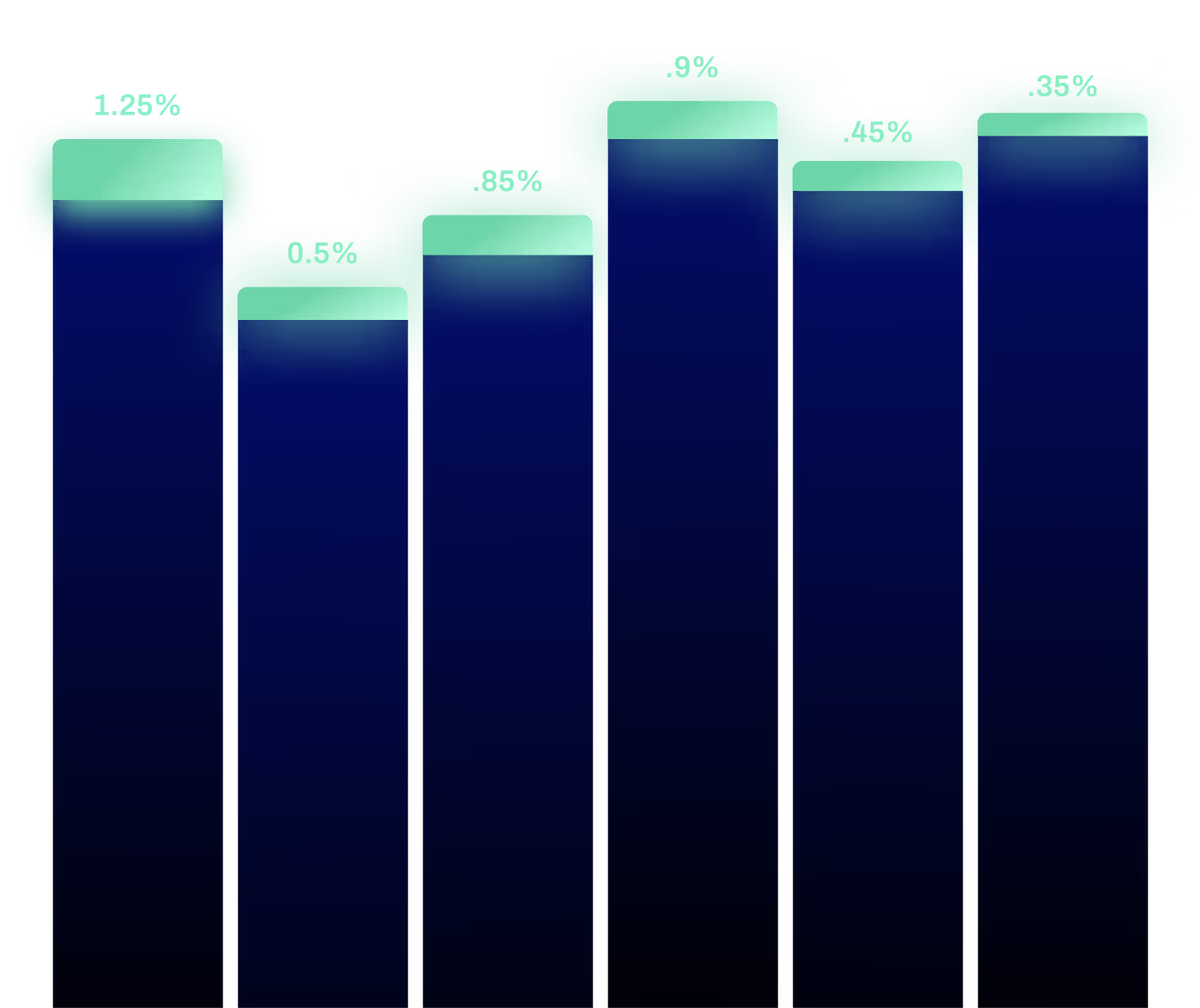
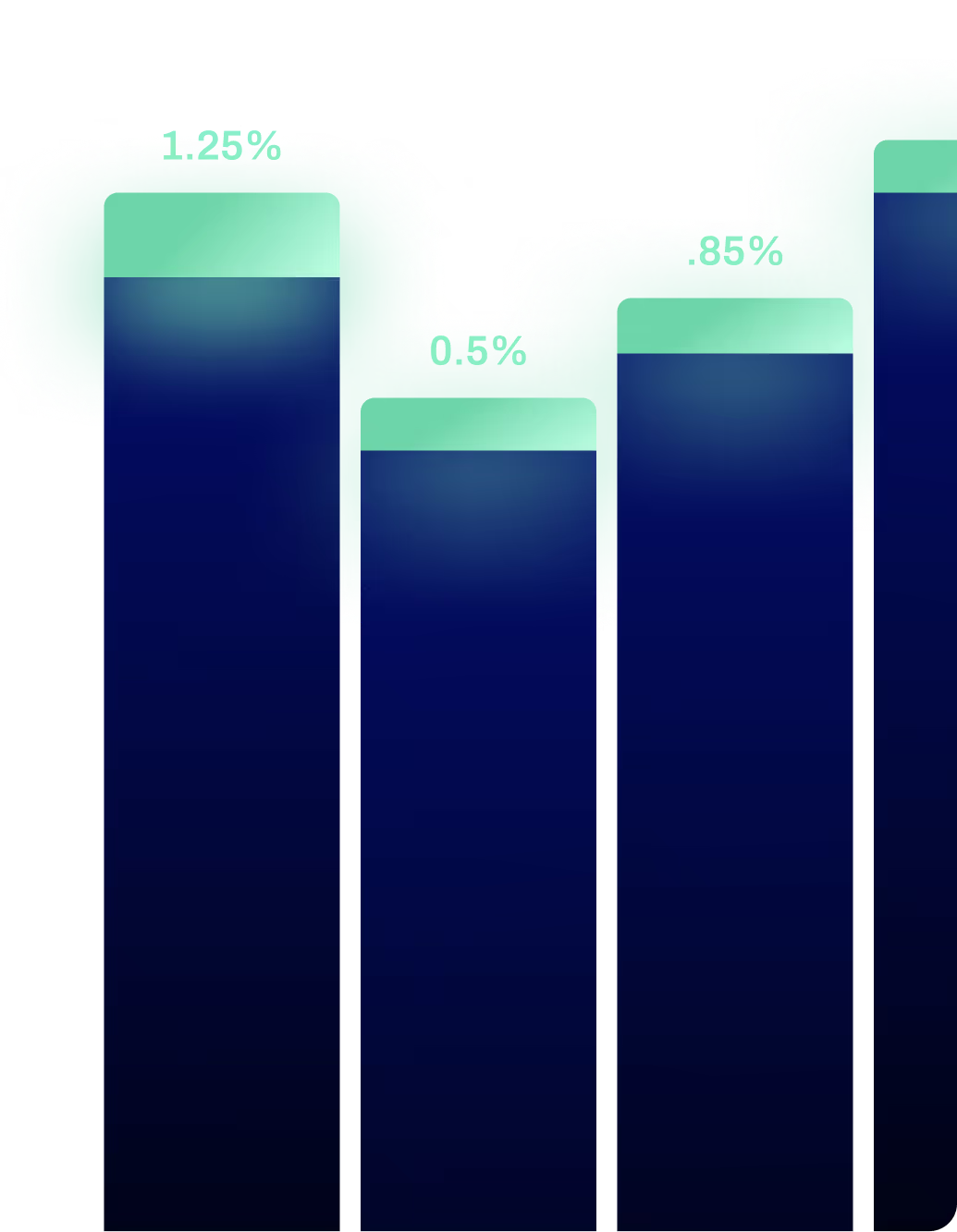
Even high performing CDI teams can’t review every data point of every chart — no human can.
Even if hypothetically, a CDI team achieved 99.5% chart accuracy, that remaining .5% could potentially add up to millions in missed revenue for a large health system — as well as improved quality of care scores.
Many CDI teams have technology in place that prioritizes charts, but still doesn’t address all charts. No matter your team’s benchmark, AI can meaningfully help improve revenue and quality capture.

There are 30,000 data points per patient chart and 156,000+ ICD-10 codes.
It’s simply not feasible for the human eye to review that many data points for every discharge in a given shift, let alone catch every single missing or incorrect diagnosis.
Advanced clinical AI can process and analyze all of that information, then present its recommendations to CDI professionals for validation.


AI is here to make the lives of CDI teams easier, not replace them.
44% of CDI professionals did not agree that they were adequately staffed for the workload they had.2
With AI doing the analysis, CDI pros can practice at the top of their license and evaluate the most relevant information AI has identified.


Not all technology investments have to come with a big price tag.
CDI teams can explore a couple of paths here: First, look for solutions that can offer an attributable ROI.
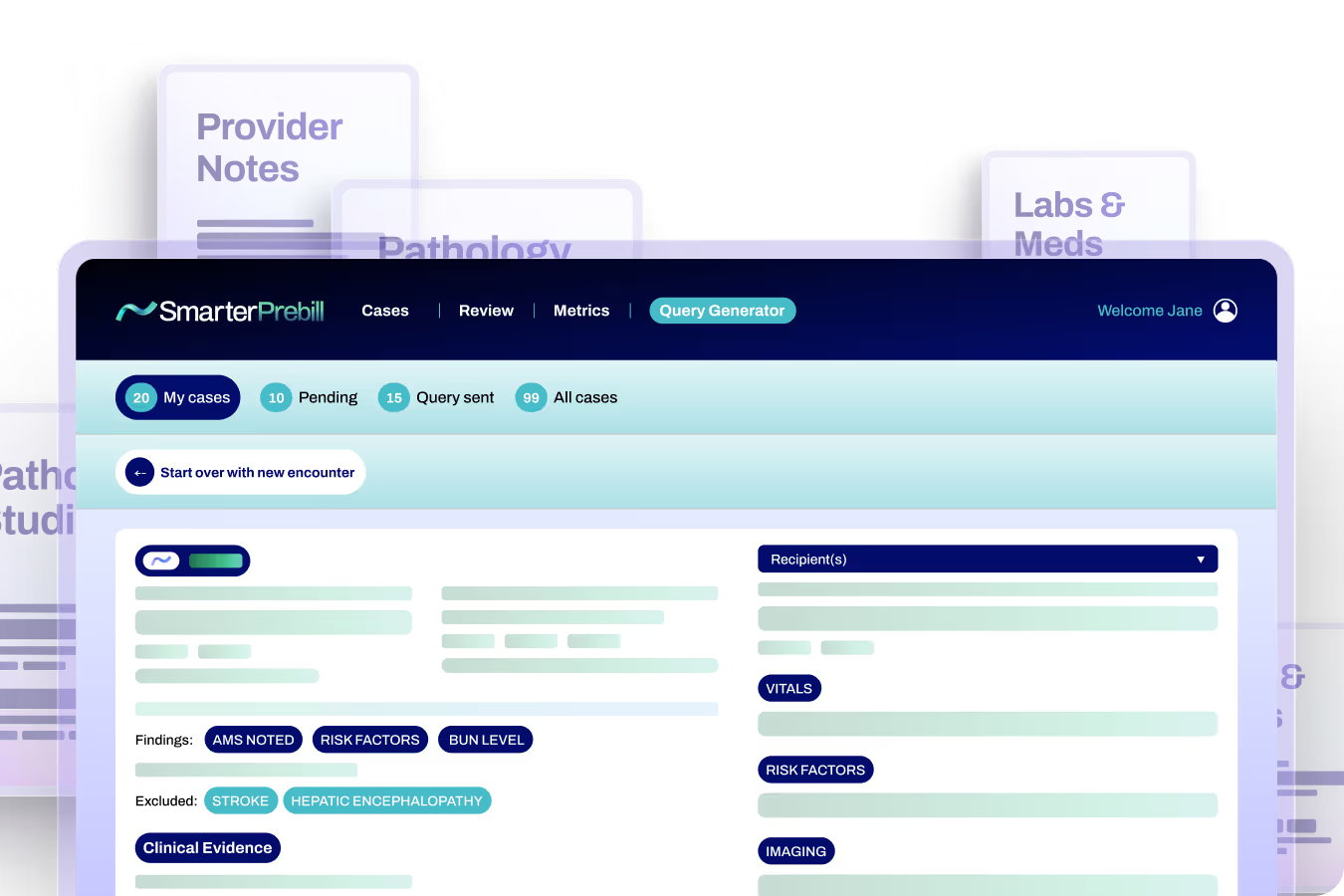
For example, explore clinical AI that sits in the prebill stage, but after your team’s CDI workflows and processes. That makes any findings directly attributable to the AI, and gives the CDI team an opportunity to approve and validate.
Second, consider new models like contingency-based models that share in risk and reward by only paying for approved and billed findings from the new revenue that is captured.
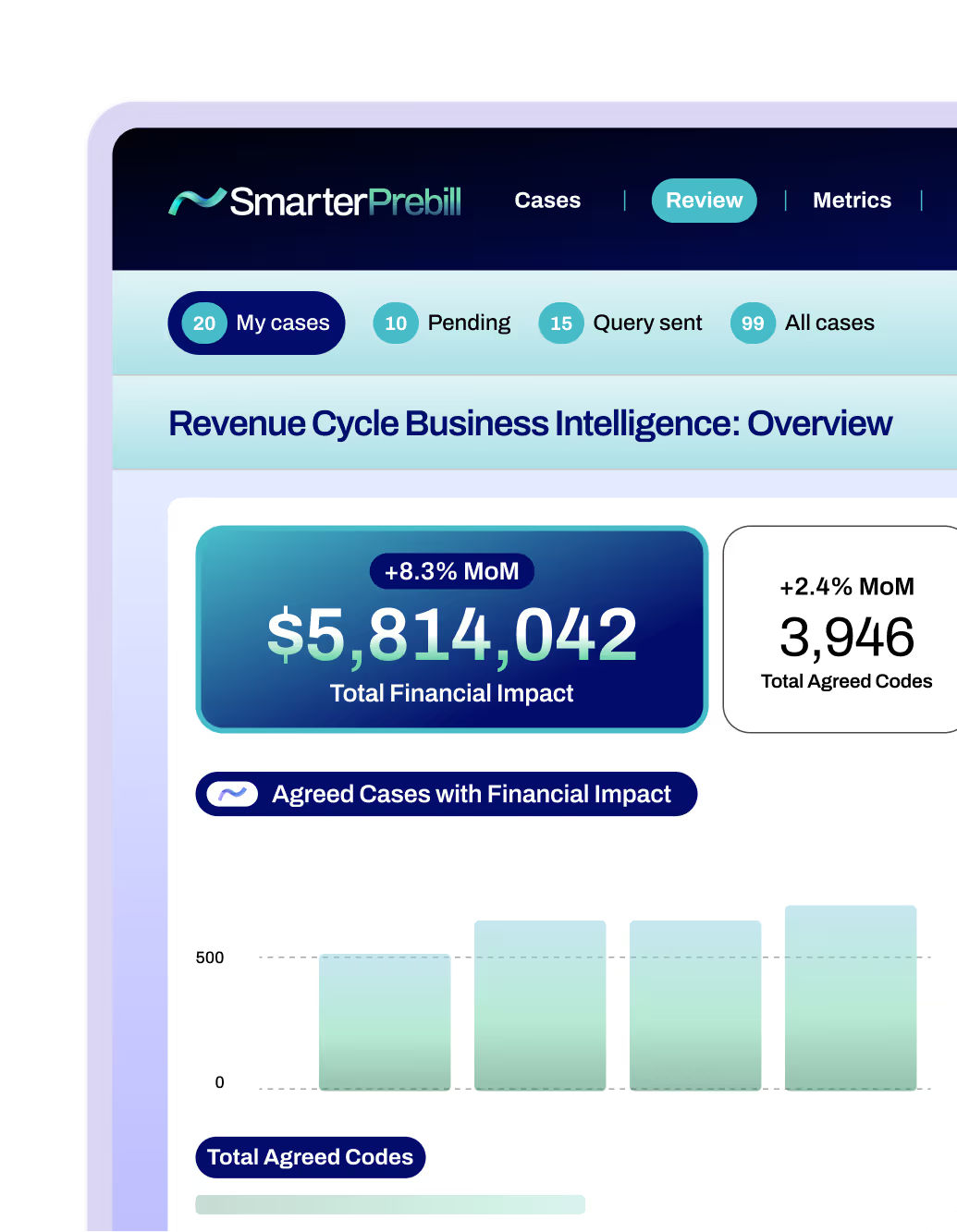

SmarterPrebill is clinical AI that helps CDI teams review 100% of patient charts to fully capture the value of the care delivered — both quality and revenue. Even with other technology and/or services in place, SmarterDx has been able to find an average of $2.5 million in realized annual net new revenue per 10,000 patient discharges for its hospital and health system clients.

1. AIPRM 50+ AI in Healthcare Statistics 2024, 2024
2. ACDIS “Industry Overview Survey” Results, 2023
Ready to learn more? Get in touch with us today and we’ll set you on the path to revenue integrity.
